
Nov. 10, 2023
First-Generation Week: Jayde Sharp
From a small-town high school where she worked extra hard to get ahead, to carrying the prestige of five degrees as a first-generation student – one word best describes Jayde Sharp, Unstoppable.
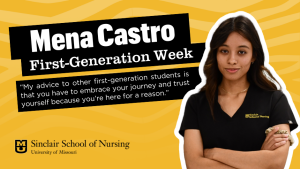
Nov. 7, 2023
First-Generation Week: Mena Castro
Immigrant parents inspire and motivate first-generation daughter to overcome challenges
Oct. 18, 2023
Faculty Spotlight: Dr. Ellen Chiocca
Dr. Chiocca has devoted 41 years to being a nursing crusader.

Oct. 17, 2023
SSON Graduate Student to Compete in Mizzou Entrepreneur Quest 2023
Sinclair School of Nursing Dean Lori Popejoy, right, celebrates with nursing doctoral candidate Lauren Compton at last month's pitch competition. Compton was chosen as the audience favorite and won $2,000 from Hawthorn Bank.

Oct. 9, 2023
Anne Sales – The Implementer
Anne Sales is building capacity in an emerging field that has tremendous potential to improve patient care and public health.

Sep. 12, 2023
SSON home to first Lifecast Manikin at Mizzou
Hyper-realistic geriatric manikin takes training for Mizzou nurses to a new level

July 13, 2023
Faculty Spotlight: Dr. Gina Oliver
Dr. Oliver, one of Mizzou Nursing's most prominent educators, has devoted her career to educating future nurse educators.

June 2, 2023
Student Spotlight: Emma Morrow
Up-and-coming Mizzou Nursing student and researcher, says, "Both the entire nursing profession, as well as nurse researchers, have one goal in mind: to aid others in every way possible."

May 13, 2023
Josie Woodward – Graduate Spotlight
Golden Girl dances her way through Mizzou Nursing to the Pulmonary ICU.

May 9, 2023
Luke Pfitzinger – Graduate Spotlight
Pfitzinger, a Mizzou Nursing legacy, volunteer firefighter, EMT and Columbia local, plans to stay with the University of Missouri Hospital after commencement.