Recent News

Oct. 9, 2025
Welcome Nelda Godfrey, PhD, ACNS-BC, FAAN, ANEF
Sinclair School of Nursing Welcomes Dr. Nelda Godfrey as Professor of Professional Practice and Director of Nursing Career Success, Identity and Innovation
Sep. 17, 2025
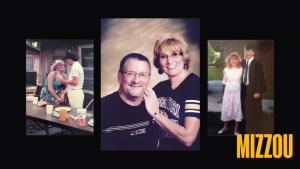
Mizzou business alum reflects on legacy of late wife, nursing alum
A bequest divided between the Sinclair School of Nursing and the Trulaske College of Business serves a fitting tribute to an unwavering partnership between graduates of the two academic units.

Aug. 14, 2025
Mizzou nursing students make lasting impact on summer campers
As part of their community health clinical rotation, Sinclair School of Nursing students spent the summer delivering hands-on care to individuals with special needs at camp.

May 13, 2025
Nursing graduate follows in black and gold footsteps
The youngest of four siblings who all attended Mizzou, Mary Grace Cantalin plans to graduate this spring and return to St. Louis to work as an ER nurse.

May 13, 2025
Whitt explores her interests — and the world — at Mizzou
After studying and serving others in Italy, Jamaica and Japan, Abigail Whitt will graduate this spring and start working in Mizzou’s University Hospital, where her parents met.

Dec. 19, 2024
A Legacy of Care: Michele Herndon’s Journey of Resilience and Advocacy
Michele Herndon graduated in December with her Doctor of Nursing Practice (DNP) at the Sinclair School of Nursing. Long before she walked across the stage at Jesse Auditorium, she dedicated her life to transforming health care systems and improving patient outcomes. Michele’s story is one of resilience, innovation and honoring her son Mitchell’s legacy.

Dec. 13, 2024
Leaving a legacy of happiness
Mizzou nursing graduate Christian Birtell is showing that a positive attitude can be contagious at the Show Me State’s flagship university, and his newly created “Show Me Happy” student organization will live on as he starts his nursing career at MU Health Care.


